Proven Clinical Experience
Proven Clinical Experience
Prescription drug candidates today go through clinical trials and rigorous efficacy and safety testing but what does that mean for its use in the real world? What does that mean for you?
Clinical studies are very important for bringing products to market, and for expanding the indications for current products. At any given time there are a number of clinical studies happening in hemophilia with the goal of bringing you safe and efficacious drugs. Please read below about one drug and its clinical study results.
Indications
ADVATE is a medicine used to replace clotting factor (factor VIII or antihemophilic factor) that is missing in people with hemophilia A (also called “classic” hemophilia).
ADVATE is used to prevent and control bleeding in adults and children (0-16 years) with hemophilia A.
Your healthcare provider may give you ADVATE when you have surgery.
ADVATE can reduce the number of bleeding episodes in adults and children (0-16 years) when used regularly (prophylaxis).
ADVATE is not used to treat von Willebrand disease.
SELECTED IMPORTANT RISK INFORMATION
You should not use ADVATE if you:
• Are allergic to mice or hamsters.
• Are allergic to any ingredients in ADVATE.
Tell your healthcare provider if you are pregnant or breastfeeding because ADVATE may not be right for you.
Extensively Studied
ADVATE has been extensively studied, with results spanning over a decade.1-6
In one study it was shown that:
• 42% of patients experienced zero bleeds during one year on prophylaxis7
• prophylaxis with ADVATE improved physical health-related quality of life compared with on-demand treatment7*
*Clinically meaningful changes were not seen in the physical health-related sub-categories of General Health and Physical Functioning, and the mental health-related component score and sub-categories of Mental Health, Role Emotional, Social Functioning, and Vitality.
We’re proud that only ADVATE has 13 years of real-world experience as a third-generation plasma/albumin-free recombinant factor VIII and it has physical health-related quality-of-life results in the prescribing information for people with hemophilia A.7,8
SELECTED IMPORTANT RISK INFORMATION
Your body may form inhibitors to factor VIII. An inhibitor is part of the body’s normal defense system. If you form inhibitors, it may stop ADVATE from working properly. Consult with your healthcare provider to make sure you are carefully monitored with blood tests for the development of inhibitors to factor VIII.
Side effects that have been reported with ADVATE include: cough, headache, joint swelling/aching, sore throat, fever, itching, unusual taste, dizziness, hematoma, abdominal pain, hot flashes, swelling of legs, diarrhea, chills, runny nose/congestion, nausea/vomiting, sweating, and rash.
Tell your healthcare provider about any side effects that bother you or do not go away or if your bleeding does not stop after taking ADVATE.
Our Commitment
Shire is committed to advancing treatment and providing product support programs and services for patients like you. Learn more about our CoPay assistance program, free trial offer and so many other great resources to help you through your journey at ADVATE.com.†
†Eligibility requirements, restrictions and terms and conditions apply.
Please click here for ADVATE Indications and Detailed Important Information.
ADVATE [Antihemophilic Factor (Recombinant)] Important Information
Indications
ADVATE is a medicine used to replace clotting factor (factor VIII or antihemophilic factor) that is missing in people with hemophilia A (also called “classic” hemophilia).
ADVATE is used to prevent and control bleeding in adults and children (0-16 years) with hemophilia A.
Your healthcare provider may give you ADVATE when you have surgery.
ADVATE can reduce the number of bleeding episodes in adults and children (0-16 years) when used regularly (prophylaxis).
ADVATE is not used to treat von Willebrand disease.
DETAILED IMPORTANT RISK INFORMATION
You should not use ADVATE if you:
• Are allergic to mice or hamsters.
• Are allergic to any ingredients in ADVATE.
Tell your healthcare provider if you are pregnant or breastfeeding because ADVATE may not be right for you.
You should tell your healthcare provider if you:
• Have or have had any medical problems.
• Take any medicines, including prescription and non-prescription medicines, such as
over- the-counter medicines, supplements or herbal remedies.
• Have any allergies, including allergies to mice or hamsters.
• Have been told that you have inhibitors to factor VIII (because ADVATE may not
work for you).
Your body may form inhibitors to factor VIII. An inhibitor is part of the body’s normal defense system. If you form inhibitors, it may stop ADVATE from working properly. Consult with your healthcare provider to make sure you are carefully monitored with blood tests for the development of inhibitors to factor VIII.
You can have an allergic reaction to ADVATE.
Call your healthcare provider right away and stop treatment if you get a rash or hives, itching, tightness of the throat, chest pain or tightness, difficulty breathing, lightheadedness, dizziness, nausea or fainting.
Side effects that have been reported with ADVATE include: cough, headache, joint swelling/aching, sore throat, fever, itching, dizziness, hematoma, abdominal pain, hot flashes, swelling of legs, diarrhea, chills, runny nose/congestion, nausea/vomiting, sweating, and rash. Tell your healthcare provider about any side effects that bother you or do not go away or if your bleeding does not stop after taking ADVATE.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch, or call 1-800-FDA-1088.
Click here for ADVATE full Prescribing Information.
References:
1. Valentino LA, Mamonov V, Hellmann A, et al. A randomized comparison of two prophylaxis regimens and a paired comparison of on–demand and prophylaxis treatments in hemophilia A management [published correction appears in J Thromb Haemost. 2012;10(6):1204]. J Thromb Haemost. 2012;10(3):359–367.
2. Shapiro AD, Schoenig-Diesing C, Silvati-Fidell L, Wong WY, Romanov V. Integrated analysis of safety data from 12 clinical interventional studies of plasmaand albumin-free recombinant factor VIII (rAHF-PFM) in haemophilia A. Haemophilia. 2015;21(6):791–798.
3. Tarantino MD, Collins PW, Hay CR, et al, and the RAHF–PFM Clinical Study Group. Clinical evaluation of an advanced category antihaemophilic factor prepared using a plasma/albumin–free method: pharmacokinetics, efficacy, and safety in previously treated patients with haemophilia A. Haemophilia. 2004;10(5):428–437.
4. Négrier C, Shapiro A, Berntorp E, et al. Surgical evaluation of a recombinant factor VIII prepared using a plasma/albumin–free method: efficacy and safety of ADVATE in previously treated patients. Thromb Haemost. 2008;100(2):217–223.
5. Blanchette VS, Shapiro AD, Liesner RJ, et al, for the rAHF–PFM Clinical Study Group. Plasma
and albumin–free recombinant factor VIII: pharmacokinetics, efficacy and safety in previously treated pediatric patients. J Thromb Haemost. 2008;6(8):1319–1326.
6. Auerswald G, Thompson AA, Recht M, et al. Experience of Advate rAHF–PFM in previously untreated patients and minimally treated patients with haemophilia A. Thromb Haemost. 2012;107(6):1072–1082.
7. ADVATE Prescribing Information.
8. Grillberger L, Kreil TR, Nasr S, Reiter M. Emerging trends in plasma-free manufacturing of recombinant protein therapeutics expressed in mammalian cells. Biotechnol J. 2009;4(2):186–201.
© 2017 Shire US Inc., Lexington, MA 02421. All rights reserved. 1-800-828-2088.
SHIRE and the Shire Logo are registered trademarks of Shire Pharmaceutical Holdings Ireland Limited or its affiliates.
ADVATE is a trademark or registered trademark of Baxalta Incorporated, a wholly owned, indirect subsidiary of Shire plc.
All other product brands or trademarks appearing herein are the property of their respective owners
S32465 07/17




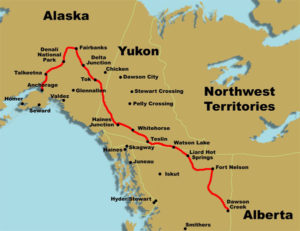 With only five days and 250 miles to go, Barry Haarde is entering the final stretch of his Wheels for the World bike tour to raise funds for Save One Life.
With only five days and 250 miles to go, Barry Haarde is entering the final stretch of his Wheels for the World bike tour to raise funds for Save One Life. What’s remarkable about this achievement is that Barry has hemophilia, HIV and a contracted knee joint… health issues that would stop most people from considering this audacious ride. But Barry is not most people…he’s driven by memories of the brother and brother-in-law he lost to hemophilia and HIV, and all the friends in the community lost to HIV. In addition, he knows firsthand the pain suffered by those in developing countries who often lack access to blood-clotting medicine.
What’s remarkable about this achievement is that Barry has hemophilia, HIV and a contracted knee joint… health issues that would stop most people from considering this audacious ride. But Barry is not most people…he’s driven by memories of the brother and brother-in-law he lost to hemophilia and HIV, and all the friends in the community lost to HIV. In addition, he knows firsthand the pain suffered by those in developing countries who often lack access to blood-clotting medicine. Thank you, Barry!
Thank you, Barry!
