FAQs
We know you have questions about hemophilia and bleeding disorders. That’s why we’ve rounded up the most popular ones and answered them in detail.
Hemophilia Basics
Hemophilia is a genetic bleeding disorder that prevents blood from forming an effective clot. Without an effective clot, bleeding from injuries may be prolonged or not stop. This can cause joint damage or other complications, and may be life-threatening.
Hemophilia is rare: it’s estimated that only about 20,000 people in the United States have hemophilia. Hemophilia A occurs in approximately 1 in 5,000 male births. Hemophilia B occurs in about 1 in 20,000 male births.To put this in perspective, Down syndrome occurs in 1 of every 700 births, and spina bifida occurs in 1 to 2 of every 1,000 births.
- Vasoconstriction. Muscles in the damaged blood vessel wall tighten, narrowing its diameter and reducing blood flow inside the injured vessel. Even in people with hemophilia, vasoconstriction in blood vessels may sometimes be enough to stop blood flow from small cuts.
- Platelet plug. Platelets are activated at the site of the injury, causing them to become sticky and adhere to the wound and to each other. The sticky platelets plug the hole in the blood vessel.
- Fibrin clot. The platelet plug is weak. To prevent it from breaking down and falling out, restarting the bleeding, the plug must be strengthened and held in place. This is done with fibrin, a tough fibrous substance produced by a complex reaction of plasma proteins called clotting factors. Clotting factors travel in the bloodstream.

 When anyone is cut, they bleed. People with hemophilia also bleed, although they do not “gush” blood, as is commonly believed. They are not in any greater danger of bleeding to death than anyone else. If the cut is shallow, as from a paper cut or a small razor blade cut while shaving, pressure can be applied to the wound. Pressure – placing your hand firmly on the bleeding to stop the flow of blood – pinches the blood vessel wall to close off the tear. If the cut is large or deep, special medicine might have to be given to stop the bleeding.
When anyone is cut, they bleed. People with hemophilia also bleed, although they do not “gush” blood, as is commonly believed. They are not in any greater danger of bleeding to death than anyone else. If the cut is shallow, as from a paper cut or a small razor blade cut while shaving, pressure can be applied to the wound. Pressure – placing your hand firmly on the bleeding to stop the flow of blood – pinches the blood vessel wall to close off the tear. If the cut is large or deep, special medicine might have to be given to stop the bleeding.
People bleed all the time. Sometimes they don’t even realize it. You may have bumped your leg today, and you may have broken some blood vessels. Your broken blood vessels may have healed so quickly that you did not even get a bruise.
But if you have hemophilia, the bleeding may have continued at a slow and steady rate until a large “black and blue” mark developed. This may take hours. Bruising may just be bleeding under the skin. Usually this is nothing to worry about.
Some people with hemophilia have no working factor in their blood. Others with hemophilia have some working factor but not enough to stop all bleeds. Some people bleed every week, some every month, others maybe only once a year. How often a person with hemophilia bleeds depends on how much factor works in the blood. Severe hemophilia means little or no factor works in the blood. Medically it is described as less than 1% active. People with severe hemophilia tend to bleed often, sometimes once or twice a week, even with no known injury! Severe hemophilia is hardly ever fatal, however, in countries like the United States.
Moderate hemophilia means some factor works in the blood. Medically, we say between 1-4% is active. Bleeding occurs usually only after some injury, and maybe only once a month on average.
Mild hemophilia means a lot of factor works in the blood. Medically, we say 5-25% active. Bleeding sometimes doesn’t happen even after an injury. Bleeding occurs maybe only a few times a year. People with mild hemophilia need to have factor when having their teeth pulled or when having surgery.
People with severe hemophilia are known to have spontaneous bleed, bleeds that seem to have no cause. Sometimes their factor levels are so low that just normal everyday activities, like walking, running or doing chores, can cause a bleed. Spontaneous bleeds usually occur in places of the body where there is a lot of activity and stress, particularly the joints. Ankles are common sites for bleeds, because ankles bear so much of the body’s weight and absorb shocks.
People with hemophilia can have different types of hemophilia depending on which factor does not work in their blood. There are at least 13 factors in the blood. Any one of them may not work properly in someone with hemophilia. This is important to know, because different types of hemophilia require different medicines.
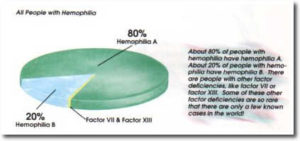
In most people with hemophilia, factor VIII is missing or does not work correctly. This is known as factor VIII deficiency or hemophilia A. Factor IX deficiency is the second most common type of hemophilia. This hemophilia is also known as hemophilia B, or “Christmas” disease.
About 80% of people with hemophilia have hemophilia A. About 20% of people with hemophilia have hemophilia B. There are people with other factor deficiencies, like factor VIl or factor XIII. Some of these other factor deficiencies are so rare that there are only a few known cases in the world.
Currently, there is no cure for hemophilia. But scientists are always trying to find a cure. They believe the answer lies in gene therapy. The chemical directions for blood clotting are found on a certain gene in each cell of the body. When you have hemophilia, the directions are scrambled, and the body can’t read them correctly. The body can’t produce enough factor that works.
To cure hemophilia, scientists hope to repair or replace the faulty gene. This could mean taking genes with the correct directions for making factor and inserting them into the cells of a person with hemophilia. Scientists believe the new gene will give the correct directions to the body to start producing high levels of factor. The person with hemophilia might now develop successful blood clotting.
Yes. Unless they find a cure, you will always have it. Some people think of hemophilia like other diseases that get better or worse, but hemophilia is more like having a finger or toe that never worked correctly from birth. The body can’t fight hemophilia like other diseases, because there is nothing to fight! Hemophilia is not a germ or infection. A protein in my blood does not work properly. Everything else works successfully in my blood and body.
It is rare, but yes! If a man with hemophilia married a woman who was a carrier then they might have a girl with hemophilia. The chances of having a girl with hemophilia would be 50%.
There are girls with hemophilia, and boys with hemophilia, whose mothers are not even carriers! Occasionally something goes wrong inside the cells of a developing baby, even when the parents have nothing wrong with them. In one-third of all cases of hemophilia, the mother is not a carrier of hemophilia! Something just went a little wrong inside the baby.
Glossary
Largest blood vessels. Arteries bring oxygenated blood from the lungs to the rest of the body.
Spontaneous bleeds that occur while a person is on prophylaxis.
Blood-clotting product that skips the steps in the clotting process where factor VIII or IX is needed. Useful for inhibitor patients, who often can’t use regular factor VIII or IX products.”
Person who has a gene for a certain trait, but who does not normally exhibit that trait.
One of several blood tests that can determine whether a female has the hemophilia gene. When she knows her carrier status, she can make more informed family planning decisions.”
Another name for hemophilia B or factor IX deficiency. Named in 1952 after Stephen Christmas, the first patient to be diagnosed with factor IX deficiency.
Structure that contains the genes within the nucleus of each cell.
Series of cellular and chemical reactions involving the 13 blood-clotting factors in response to an injured blood vessel. Ends with the formation of fibrin fibers in the platelet plug, forming a blood clot.
Formation of a blood clot.
A genetic carrier test. The hemophilia gene of an affected male is examined to determine the exact location and nature of the mutation that caused hemophilia in that person. If a specific mutation is identified, relatives can be screened to identify carrier status because the exact location of the mutation is known. A woman with the mutation is a carrier.
Molecule that codes for how living organisms are built. Segments of DNA that give traits to offspring are called genes.
Proteins that are catalysts (capable of initiating or accelerating chemical reactions without being consumed).
Medical treatment for hemophilia that involves an infusion of factor concentrate given before an activity such as a sporting event or extended travel.
1. One of the 13 blood proteins that help clot blood. 2. Informal term for any commercially prepared factor concentrate infused to replace the body’s missing or inactive factor.
Commercially prepared freeze-dried factor that is reconstituted with water or saline and infused to treat bleeding that results from factor deficiency.
Strong sheets of connective tissue.
Protein required for blood clotting. Forms a net of fibers that hold blood platelets together in a clot, the end result of the clotting cascade.
Single unit of heredity. A segment of DNA that carries information for functional products such as proteins and is responsible for physical and inheritable traits of an organism such as hair color and eye color. Mutations (changes) to genes may cause genetic disorders such as hemophilia. Genes are sequences of DNA located in string-like groups called chromosomes, found in each cell.
Procedure in which normally functioning genes can be inserted into a patient’s own cells; in turn, those cells produce the specific protein controlled by the particular genes. Gene therapy is one area of research for a cure for hemophilia.
Inherited.
Permanent change in a gene that scrambles the instructions carried by the gene. Hemophilia is a genetic mutation that scrambles the instructions for producing a blood-clotting protein such as factor VIII or IX.
Tissue bleed; bruise.
Physician who studies the nature, function, and diseases of the blood.
Presence of blood in the urine.
Any of several blood-clotting disorders in which excessive bleeding occurs because of the absence or abnormality of one of 13 clotting proteins called clotting factors.
Blood-clotting disorder in which the factor VIII protein is missing or inactive.
Blood-clotting disorder in which the factor IX protein is missing or inactive.
Form of chronic arthritis in a person“their homes, and can include a specialty pharmacy to distribute factor concentrate.
Therapy for inhibitor patients that requires high, frequent doses of factor concentrate to desensitize the body to factor VIII or IX infusions in the hope that, over time, the body may “learn” to recognize factor.
Frequency with which a disease or disorder appears in a certain population. Example: the incidence of hemophilia A is approximately 1 in 5,000 male births.
Process of injecting reconstituted factor concentrate or another drug into the bloodstream through a vein.
Classification of hemophilia in which the level of active factor is between 6% and 50%.
Classification of hemophilia in which the level of active factor is 1% to 5%.
Liquid part of blood. Contains factors VIII and IX, and von Willebrand factor.
Term used to describe factor concentrate made from human blood plasma.
Plate-shaped cell fragments in the bloodstream that create a plug over an injury site in a blood vessel wall. Platelets are essential for blood clotting.
The sticky accumulation of platelets that occurs when platelets are activated at the site of a blood vessel injury as the body attempts to stem bleeding. One step in the coagulation process.
Central venous access device surgically implanted under the skin, typically in the chest wall, to facilitate IV infusions. SEE CENTRAL VENOUS ACCESS DEVICE.
Person who may carry a gene for a specific trait, such as hemophilia. Possible carriers in hemophilia include mothers of children with hemophilia who have no history of hemophilia in the family and daughters of carrier mothers.
Medical testing done during pregnancy, often to check for genetic disorders or birth defects.
Number of cases of a disorder or disease present in a given population at a certain time. The prevalence of people with hemophilia in the United States is estimated to be about 20,000.
Medical treatment for hemophilia that involves scheduled infusions of factor concentrate before any joint damage occurs, and sometimes even before any bleeds occur, usually in infancy.
Describes commercial recombinant factor concentrate modified to maintain clotting activity for an extended period past the normal half-life of the particular factor.
Blood plasma without clotting factors.
Hemophilia classification system based on the percentage of normal factor active in the blood. There are three severity levels: severe, moderate, and mild. Severe hemophilia: less than 1% of factor is active. Moderate hemophilia: 1% to 5% of factor is active. Mild hemophilia: more than 6% to 50% of factor is active. Normal factor activity is considered to be between 50% and 150%, with most people near 100%.
Licensed distributor of biologic products such as factor concentrates.
Free of microorganisms. Examples: surgical instruments, infusion needles, and syringes are sterile before the package is opened.
Carrier who exhibits excessive bleeding. Symptomatic carriers essentially have hemophilia and risk excessive bleeding during dental extraction, surgery, or childbirth, and may have frequent nosebleeds, bruising, and heavy menstrual bleeding.
Blood vessels that bring blood back to the heart from all parts of the body. IV medications are typically infused into veins.
Most common inherited bleeding disorder. Caused by low levels of von Willebrand factor (VWF) or malfunctioning VWF; results in platelets not sticking together during blood clotting. Symptoms include prolonged bleeding, nosebleeds, soft tissue bleeds, menorrhagia, gastrointestinal bleeds. VWD affects men and women equally, but is diagnosed more often in women because of bleeding problems in childbirth and menstruation.
X-shaped chromosome that carries the gene with instructions for female development. One of the two sex chromosome, along with the Y chromosome found in males. Any gene on the X chromosome, including the hemophilia gene, is said to be X-linked.
Y-shaped chromosome that carries the gene with instructions for male development. Found only in males. Along with the X, the Y is one of the two sex chromosomes.
Lifestyle
Swimming, biking, karate, baseball, skiing…. These are just some of many activities that people with hemophilia can do. And there are few sports and activities that are not recommended for a person with hemophilia.
Which sport or activity is best? That depends on the person with hemophilia and their doctor. The decision should be based on which activity the person enjoys, what physical shape they are in and whether they have joint problems that would exclude certain activities. The important thing is to find something that interests you or that challenges your body. Exercise is important for everyone.
Most doctors agree that the roughest physical contact sports, such as boxing, hockey or football, should be avoided by people with hemophilia.
My right knee is a target joint. I had a lot of bleeds in it when I was growing up. Each time I had a bleed, blood would accumulate in my right knee joint cavity. Over time, blood can act like acid on the smooth, protective cartilage that everyone has on the ends of their bones. The blood damaged the cartilage on the ends of my upper and lower right leg bones, where they meet at the knee. The cartilage is no longer smooth, and it makes my knee stiff and causes it to bleed often.
I’m on prophylaxis. Prophylaxis means prevention. Boys and girls on prophylaxis are infused with factor up to three times a week, whether they need it or not. This keeps the factor levels high in their blood so they should not even get bleeds. There are children with hemophilia today who never experience bleeds because they are on prophylaxis! New information shows that long-term prophylaxis will help protect my joints. So when I am an adult, my joints will be in great shape. There are also new prolonged half-life factor products which require only one injection a week, in some cases. These also help protect my joints from bleeds.
Wrong! Prophylaxis is used only by some people with hemophilia. It is a very expensive medical treatment because it uses a lot of factor and factor is expensive. Some people have medical insurance that will pay for prophylaxis. Many people do not, however.
A blood transfusion would stop bleeds, but only for about 12 to 24 hours. Just as we eat and use up our food, and need to eat more, so the body also uses up factor daily and must make more. A one-time transfusion (just like a great feast) would not cure hemophilia (nor leave your stomach full forever) because the body uses up its factor (or food). This is called the half-life of factor. As the factor is used up, the genes need to send directions to the body to make more factor, to replenish the supply. People with hemophilia cannot do this. Their only hope of a cure lies in finding a way to make their bodies capable of making their own factor. Until then, they continue to depend on infusions of factor.
They may have an inhibitor. An inhibitor is an antibody to factor VIII or IX. Inhibitors develop when the immune system identifies infused factor as a foreign material and produces antibodies to inactivate the factor. An inhibitor inactivates infused factor before it has time to stop a bleed. This requires careful medical attention.
People with severe hemophilia have so little factor in their bloodstream that when factor is infused to stop a bleed, their bodies do not “recognize” the medicine as a normal substance that belongs there. The body treats the factor as an invading substance that does not belong – and tries to destroy it. Several different treatments can be tried to destroy the inhibitor. Luckily, most boys with hemophilia do not develop inhibitors.
Science of Hemophilia
- Vasoconstriction. Muscles in the damaged blood vessel wall tighten, narrowing its diameter and reducing blood flow inside the injured vessel. Even in people with hemophilia, vasoconstriction in blood vessels may sometimes be enough to stop blood flow from small cuts.
- Platelet plug. Platelets are activated at the site of the injury, causing them to become sticky and adhere to the wound and to each other. The sticky platelets plug the hole in the blood vessel.
- Fibrin clot. The platelet plug is weak. To prevent it from breaking down and falling out, restarting the bleeding, the plug must be strengthened and held in place. This is done with fibrin, a tough fibrous substance produced by a complex reaction of plasma proteins called clotting factors. Clotting factors travel in the bloodstream.

Hemophilia means that the fibrin net does not get made properly. Without the fibrin net, the platelet plug falls out and bleeding continues.
Why does this happen? With hemophilia, one of the 13 clotting factors does not work properly. When a blood vessel is torn, usually the blood vessel constricts and the platelets make a plug. The clotting factors start giving each other directions: factor III, for example, directs factor VII. But then something doesn’t work right – the directions for blood clotting. The creation of the fibrin net stops and the bleeding continues.
Anyone can start bleeding internally following a blow to the abdomen, head, arm or leg, or after a fall that injures the knee or elbow. People without hemophilia may stop bleeding and heal on their own. People with hemophilia may continue to bleed internally, slowly and steadily, sometimes for hours or even days after the injury. They may not even realize they are bleeding at first. But it is necessary to get medicine immediately. Why?
Let’s look at an example. A joint is a place where two bones meet. Inside the joint is a space called the joint cavity. This cavity allows you to move the two bones. The bone ends that meet to form the joint are protected by a smooth substance called cartilage, which covers the end of each bone like a cap.
 Now let’s imagine that someone with hemophilia falls and injures a knee. Blood steadily leaks into the joint cavity. The joint begins to swell and ache. The joint becomes stiff. The leg cannot bend, and walking becomes difficult and painful. Even worse, blood has substances in it called enzymes. Enzymes break down other substances. As blood accumulates in the joint cavity, enzymes begin to break down the blood to get it out of the joint where it does not belong, to be reabsorbed into the body. This is good. But as the enzymes do this, they also start to break down the cartilage covering the bone ends. If joint bleeds are allowed to continue for too long or happen too many times, the cartilage may become permanently rough and jagged, making smooth joint movement painful.
Now let’s imagine that someone with hemophilia falls and injures a knee. Blood steadily leaks into the joint cavity. The joint begins to swell and ache. The joint becomes stiff. The leg cannot bend, and walking becomes difficult and painful. Even worse, blood has substances in it called enzymes. Enzymes break down other substances. As blood accumulates in the joint cavity, enzymes begin to break down the blood to get it out of the joint where it does not belong, to be reabsorbed into the body. This is good. But as the enzymes do this, they also start to break down the cartilage covering the bone ends. If joint bleeds are allowed to continue for too long or happen too many times, the cartilage may become permanently rough and jagged, making smooth joint movement painful.
Muscles are also a common spot for internal bleeds. Muscles can act like sponges, and can hold a lot of blood. Muscle bleeds cause swelling and can limit movement. Luckily, there are plenty of symptoms when someone gets a joint or muscle bleed: many say these bleeds feel “tingly,” “funny” or “hot.” Medicine (or clotting factor) can help stop a bleed before there is damage to the muscle.
People with hemophilia can lead practically normal lives by using commercial prescription medicine, called factor. This medicine, injected into the veins, replaces the factor that does not work properly. With all the factors working properly, the directions for blood clotting are passed along until the fibrin net is formed.
 Factor comes in small bottles and looks like packed white powder. When properly mixed with sterile water, factor is ready to be infused – injected directly into a vein. When it is infused, factor does not go directly to the site of the bleed; it takes a trip around the body. All veins carry blood back to the heart, so factor goes back to the heart, too. Then the heart pumps factor out to all parts of the body at the same time, including the place that is bleeding. Factor can work quickly to stop a bleed.
Factor comes in small bottles and looks like packed white powder. When properly mixed with sterile water, factor is ready to be infused – injected directly into a vein. When it is infused, factor does not go directly to the site of the bleed; it takes a trip around the body. All veins carry blood back to the heart, so factor goes back to the heart, too. Then the heart pumps factor out to all parts of the body at the same time, including the place that is bleeding. Factor can work quickly to stop a bleed.
 Infants and small children with hemophilia are usually infused by doctors and nurses who are experts in hemophilia care. As a child grows older, he can be infused at home by his parents, who are trained by the doctors and nurses. Eventually the child with hemophilia can learn to infuse himself. An infusion doesn’t take long and can be done at home, at school or at work. It’s great to be able to self-infuse because a person with hemophilia can go almost anywhere and do many activities knowing that the factor he carries will help stop a bleed quickly.
Infants and small children with hemophilia are usually infused by doctors and nurses who are experts in hemophilia care. As a child grows older, he can be infused at home by his parents, who are trained by the doctors and nurses. Eventually the child with hemophilia can learn to infuse himself. An infusion doesn’t take long and can be done at home, at school or at work. It’s great to be able to self-infuse because a person with hemophilia can go almost anywhere and do many activities knowing that the factor he carries will help stop a bleed quickly.
Your eye color, hair color and texture, skin color and many of your facial features – including the shape of your nose – are physical characteristics inherited from your parents. As you grew into a baby inside your mother, you were created with special cells from your father and cells from your mother. These cells had chemical “directions” in them that told your body exactly how to develop into a baby. Because some of these cells were from your father, his directions might have told you to have blue eyes like him. Or, because some of the cells were from your mother, you might have received directions to have the same curly hair as she, not the straight hair of your father. The possible combinations of the characteristics you can inherit are endless!
Guess what else can be inherited? Diseases and physical disorders. Hemophilia is a disorder that can be inherited. It can be inherited from the mother.
 A mother who can pass hemophilia along to her baby is called a carrier. This means that inside her cells she carries directions for blood clotting that are scrambled, although her blood knows how to clot correctly. When her baby inherits the cells with the scrambled directions, the baby’s body cannot “read” the directions and his blood cannot clot. This is known as hemophilia.
A mother who can pass hemophilia along to her baby is called a carrier. This means that inside her cells she carries directions for blood clotting that are scrambled, although her blood knows how to clot correctly. When her baby inherits the cells with the scrambled directions, the baby’s body cannot “read” the directions and his blood cannot clot. This is known as hemophilia.
If the mother who is a carrier had several baby boys, it’s possible that some might not have hemophilia. Sometimes the scrambled directions are passed along; sometimes they are not. Each time the mother is pregnant with a son, it is like a flip of a coin: heads, she has a boy with hemophilia; tails, she does not. Each flip of a coin has a 50% chance of coming up heads or tails.If the mother is a carrier and the father does not have hemophilia, their daughters have a 50% chance of being a carrier. They will not have hemophilia, but they may have children with hemophilia.
When a person inherits hemophilia, he receives directions for blood clotting that are mixed up chemically. His body cannot read them, and cannot clot blood properly.
Your body is made up of trillions of individual cells. A cell is like a living building block; the smallest unit of living tissue. All human life starts as a single cell inside the mother. From the moment that the egg from the mother joined with the sperm from the father to create a new life, it was already determined that the one resulting cell would grow to be a boy or girl with or without hemophilia.
How could one cell determine all this? The answer lies in your genes. Inside that one cell are all the chemical instructions needed to direct the cell to make copies of itself and then divide in two. By dividing in two repeatedly, the cell reproduces itself until there are millions, then trillions of cells. Genes direct how all the copying and dividing will be done. Genes direct some cells to become heart cells, others to grow to be brain cells, and still others to grow to be teeth, the stomach lining, or your fingernails. Genes also direct your bodily functions: how your heart will work; perhaps how quickly you will be able to learn, or run; how your blood will clot.
 The genes of some children do not have the correct directions for blood clotting. Children with hemophilia inherit these genes from their parents. Why do some children in a family inherit these genes, yet their brothers or sisters sometimes don’t?
The genes of some children do not have the correct directions for blood clotting. Children with hemophilia inherit these genes from their parents. Why do some children in a family inherit these genes, yet their brothers or sisters sometimes don’t?
The answer to this question lies in the chromosomes. The genes are wrapped into 23 pairs of chromosomes, found in every single cell in your body. On one pair of chromosomes only lies the gene with the incorrect directions for blood clotting, which causes hemophilia. It lies on the same chromosomes used to determine if you will be a boy or a girl. These are called the sex chromosomes. This is why hemophilia is “sex linked” and why usually only boys get hemophilia. Follow closely now!
Inside the mother’s egg are 23 chromosomes, or half of the mother’s genetic characteristics. Inside the father’s sperm are 23 chromosomes, half of the father’s genetic characteristics. When the egg and sperm are joined, they give the new cell 46 chromosomes, arranged in 23 pairs, exactly what is needed to begin growth from a cell to a baby.
 Will this new life be a boy or a girl? The last pair of the 23 pairs will determine this. Under a microscope, the sex chromosomes of a girl look like “XX.” The sex chromosomes of a boy look like “XY.” Whether it’s a boy or a girl, you see that there is always at least one X chromosome present. The mother’s egg always carries an X chromosome. But the father’s sperm can carry either an X or a Y chromosome. When the egg and sperm meet and begin a new life, the egg already has an X, but the sperm may give an X to make a girl or a Y to make a boy. It is the father who always determines the sex of the baby!
Will this new life be a boy or a girl? The last pair of the 23 pairs will determine this. Under a microscope, the sex chromosomes of a girl look like “XX.” The sex chromosomes of a boy look like “XY.” Whether it’s a boy or a girl, you see that there is always at least one X chromosome present. The mother’s egg always carries an X chromosome. But the father’s sperm can carry either an X or a Y chromosome. When the egg and sperm meet and begin a new life, the egg already has an X, but the sperm may give an X to make a girl or a Y to make a boy. It is the father who always determines the sex of the baby!
 Although the father’s chromosomes determine the sex of the baby, the mother’s chromosomes determine whether the baby will have hemophilia. The gene with the scrambled directions for blood clotting (hemophilia) is found only on the X chromosome. If the mother is a carrier of hemophilia, then half of all her X chromosomes have on them the scrambled instructions for blood clotting. The other half has clear directions for blood clotting. The clear directions, even if they are only on half her chromosomes, are enough to allow the mother to have normal blood clotting. This is why she does not have hemophilia.
Although the father’s chromosomes determine the sex of the baby, the mother’s chromosomes determine whether the baby will have hemophilia. The gene with the scrambled directions for blood clotting (hemophilia) is found only on the X chromosome. If the mother is a carrier of hemophilia, then half of all her X chromosomes have on them the scrambled instructions for blood clotting. The other half has clear directions for blood clotting. The clear directions, even if they are only on half her chromosomes, are enough to allow the mother to have normal blood clotting. This is why she does not have hemophilia.
But she is a carrier, so her son might receive from her the X chromosome with the scrambled directions. This is why a mother who is a carrier has a 50% chance of having a son with hemophilia. She might donate an egg with either an X chromosome affected by hemophilia or one not affected by hemophilia. This is also why her daughter might be born a carrier. The daughter might receive an affected X from her mother, but an unaffected X from her father (whose X chromosomes are all unaffected). She would not have hemophilia because the X chromosome from her father would still contain the clear directions for blood clotting.
When a boy with hemophilia, who has an affected X chromosome, grows up and has children, he will give either his X or his Y chromosome to each of his children and will determine their sex. If he gives an X chromosome to create a girl, it will have to be the one with scrambled directions for blood clotting, because, having hemophilia, all of his X chromosomes are affected. All his daughters will be carriers.