Does Hemophilia Mean Brittle Bones? Part 2
By Paul Clement
In part one of this two-part series on bone health, we discussed osteoporosis and how it causes bones to become weak and brittle. We also reviewed some risk factors for developing osteoporosis—and having a bleeding disorder is a risk factor for developing osteoporosis. But just because you have bleeding disorder does not mean you are destined to develop osteoporosis—you can do many things to lower the risk of developing osteoporosis or to lessen its severity.1
So, what can you do? First, if you smoke, stop! If you drink several alcoholic beverages or three or more cola soft drinks a day, reduce your consumption of these beverages. Eat a healthy diet containing adequate amounts of calcium and vitamin D. (Many people are deficient in vitamin D, which helps the body absorb and retain calcium and phosphorus. Check online for daily calcium and vitamin D requirements and recommended foods). And exercise!
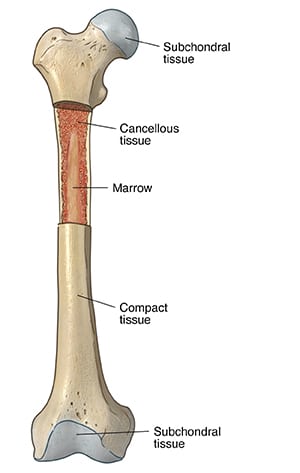
Bone growth changes in response to stress and strain applied to the bones. If you are sedentary, such as sitting around all day or sitting in an office, your bones are not subjected to regular mechanical stress. So the remodeling process tilts towards resorption and bone loss occurs. The opposite is also true. When bones are subjected to regular stress or mechanical loading, such as when walking or running, then over time, the remodeling process tilts towards new bone formation, which keeps your bones healthy and can help prevent, delay, or reduce the severity of osteoporosis.
Exercise is key! Healthy lifestyle choices are important, but they alone cannot prevent osteoporosis unless you add exercise. And not just any exercise routine—although swimming and bicycling tone muscles and provide a great cardio workout and are often recommended for people with hemophilia, they do not stress the bones sufficiently to promote new bone formation. To develop and maintain healthy bones you need to engage in regular weight-bearing exercise, such as brisk walking, dancing, aerobics, stair climbing or jogging as well as resistance exercises such as light weight lifting or use of elastic bands. (Resistance exercises are especially important for bones of the upper body, including the arms and shoulders.) Note that higher-impact weight-bearing activities, such as brisk walking or jogging, provide more benefit to bone health than lower-impact activities, such as a leisurely stroll. And although exercise is crucial in maintaining bone health throughout your lifetime, the greatest benefit is seen in childhood through age 20, when the skeleton is more responsive to exercise than in adulthood and old age, when bones become less sensitive to exercise. Greater bone strength when you are young pays lifetime benefits in the form of greater bone strength over a lifetime.
So, if you have a teenager who likes to watch TV or play video games for hours on end, get them outside and exercising. If they don’t play sports, give them chores that make them walk or carry things. Walking the dog works! Their bones will thank you!
Of course, if you have not engaged in any exercise for a while or have painful joints, you should discuss your health status with your healthcare provider before starting any new exercise program. A physical therapist associated with a hemophilia treatment center is an excellent resource to help you get started.
- There are no outward signs that you have osteoporosis—until you break a bone. The U.S. Preventive Services Task Force recommends screening for osteoporosis in women 65 years or older and men age 70 years and older, and anyone who has broken a bone after age 50 years. However, if you have hemophilia, you may already be on the path to osteoporosis in your 30s. Because of this, it is often recommended that people with hemophilia have a bone density scan earlier rather than later. (A bone density scan is a simple and fast procedure which measures bone mineral density using a special type of X-ray scan called dual energy X-ray absorptiometry, or DEXA scan.)