Zimbabwe: The Patients’ Plight
Zimbabwe is seven hours ahead of Boston, my home, but decades behind in development. Today was a sampling of a day in the life of an average Zimbabwean: long lines at the bank; money inaccessible at the bank; fears of not procuring gas for the car; telephone lines down; blackouts; and no restaurants at which to eat! Worst of all for those with hemophilia, no factor VIII, except for the stash I brought with me to donate. I am amazed at the struggles Zimbabweans must endure daily, and how graciously they accept their difficulties, how they laugh over it, even when they are most worried.
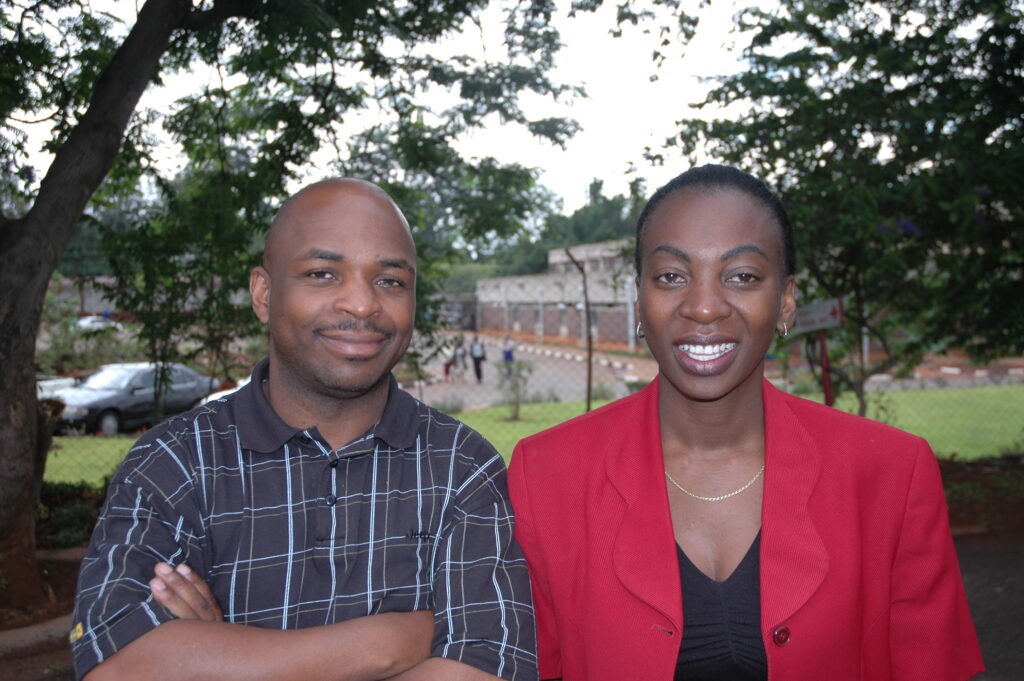
I am privileged to work with an incredible group of people: the Executive Committee of the Zimbabwe Haemophilia Association. Today was our day to brainstorm next steps in the organization. The ZHA has had rough times in recent years, not only from the economic climate but also from internal difficulties. Those times are behind them now, and the new committee is dedicated, hard working and forward looking. Members include: Simbarashe Maziveyi; Collin Zhuwao; Frankie Mutandwa; Doreen Machona; Caryn Thomas; and Peter Dhlamini. Doreen and Caryn are mother of sons with hemophilia, and the others are all young men with hemophilia. All work as volunteers.
First we met with Dr. David Mvere, CEO, and Emmanuel Masvikeni, Blood Procurement Manager, of the National Blood Service, which handles all blood donations and diagnostics for Zimbabwe. The NBS supports the ZHA as much as possible, and today’s meeting affirmed ways they can work together. Many great ideas were generated. Critical, according to Mvere, is the need to get assay kits to be able to diagnose factor deficiencies. The NBS currently cannot diagnose anyone in the country; and sitting just in the next building, at ZHA headquarters, was a young mother with a one year old covered in bruises. The woman’s brother is a diagnosed person with factor VIII; the baby is suspect but there is no way to be sure. Plans were made to try to secure kits for the NBS.
Later in the afternoon, we met at the NBS conference room to discuss ZHA needs, and set goals and prioritize them. We also discussed the option to have a board of directors, changing the constitution if needed, and ways to attract patients to the monthly meetings. The outcome was exciting, and my company has pledged to donate funds to purchase a new refrigerator for storing factor (the current one does not work) and to purchase stationery and business cards so the ZHA can start fund raising and networking. Many more plans were made for later in the year, but small steps first are best.
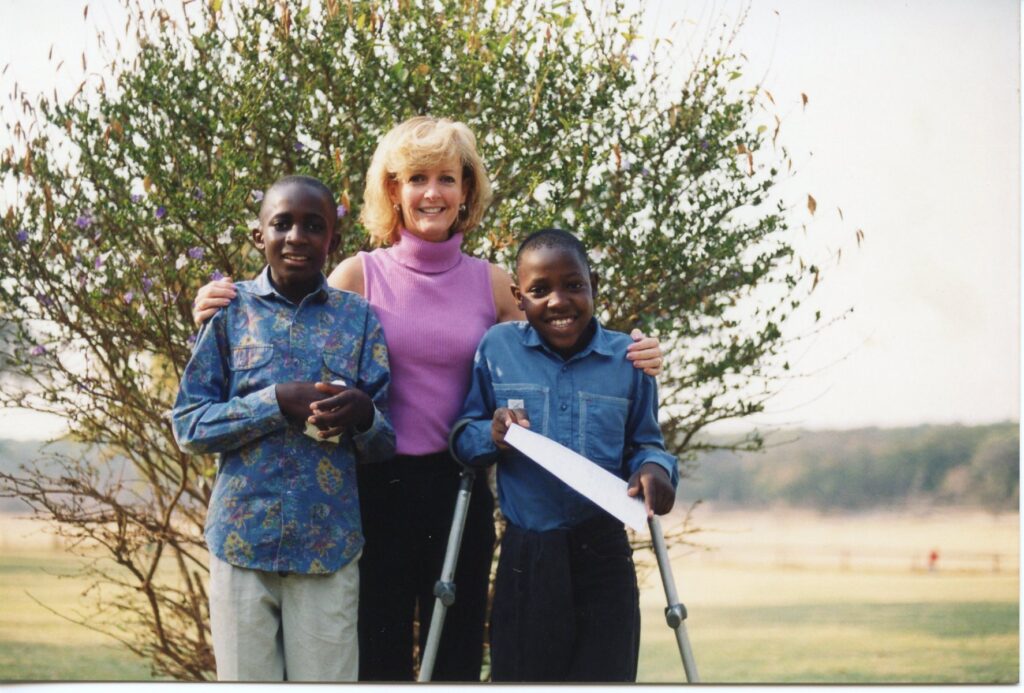
We then set out for a long ride to the outskirt of Harare to visit patients. This is always the best part of my overseas trips: to enter patients’ homes, meet the family, take in their surroundings, learn first hand what their lives are like. How can I possibly understand their needs with a compassionate heart if I don’t visit their homes? And no matter the country, families are always so honored and happy to have guests. In Zimbabwe, the traditional greeting is to clap hands, and the guest claps back, all the while saying “Makadee,” Shona for “How are you?” It was delightful! In the first home, we met Elton, age 17, and his brother Emmanuel, age 14. I changed my mind from what I previously wrote: Elton has the worst case of synovitis I have ever seen. The photo speaks for itself. He has been like this for one year. A talented student, he has had to drop out of school because he cannot walk. He is in constant pain, but like all Zimbabweans, bears it regally. I was so shocked by his condition, I discussed with Simba what we could do to help him. He needs immediate medical care. But what? To bring him to a hospital, Simba explained, would accomplish nothing. Medical staff cannot to synovectomies here. He would need to travel to South Africa. Most alarmingly, Elton’s lower leg is numb: the hideously swollen joint is compressing his nerves and blood vessels. Without intervention, it would be a matter of time before gangrene might set in. Then his leg would need to be amputated. We vowed to do something immediately to help.
We then visited Doreen’s home, and met with her family, including her son with hemophilia. Charming and chatty, he asked me, “How’s your child with hemophilia?” I was surprised to know he reads about my child from my newsletters. We sat around for a while by candlelight, as yet another black out plunged the neighborhood into darkness. 
The weather is lovely, though there are plenty of mosquitoes at night down the dusty roads we traveled. The blackouts create some suspense, as we never know quite where we are driving or walking!
The last home we visited, around 9 pm, was that of the relatives of the Norman Mubaiwe, the ZHA’s founder and my friend. Norman was the first person to contact me, back in 1997, and we became friends and colleagues. Sadly, he died on the operating table in May 2001. How happy I was to again see Daisy, his cousin, and her son with hemophilia. Daisy’s mother was a hoot, boldly asking me “How old are you?” and then sharing how her grandson showed signs of a head bleed one day, and how she turned to my book to diagnose him. She took him to the hospital, where doctors at first did not believe her. Only through her bulldog advocating, and backed by the symptoms listed in “Raising a Child With Hemophilia,” did the doctors back down, and the child was treated. Amazing example of the power of education, even in an underdeveloped country like Zimbabwe, by a simple grandmother in a rural area!
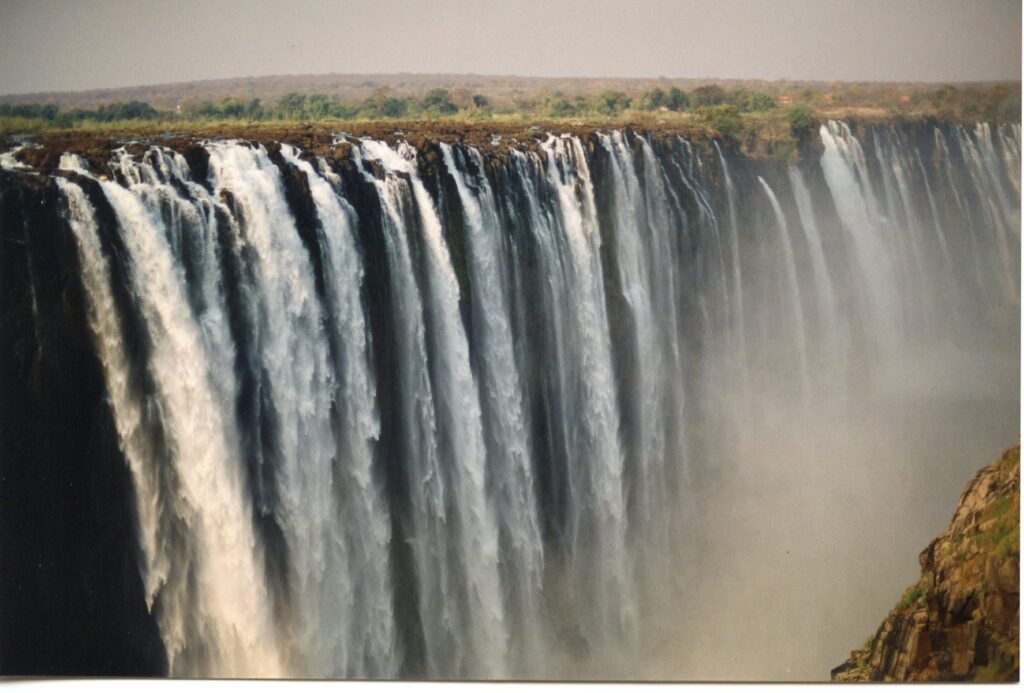
We had many hugs and clapping when we left, and promised to see one another again. Driving away in the dark, back to Harare, back to the comfortable hotel, I thought about how differently we ended our days. While the families are so appreciative, they don’t know how much gratitude I already receive just by hearing how well they use the help we give them. On to Bulawayo!