Factor Products: Purity vs. Safety
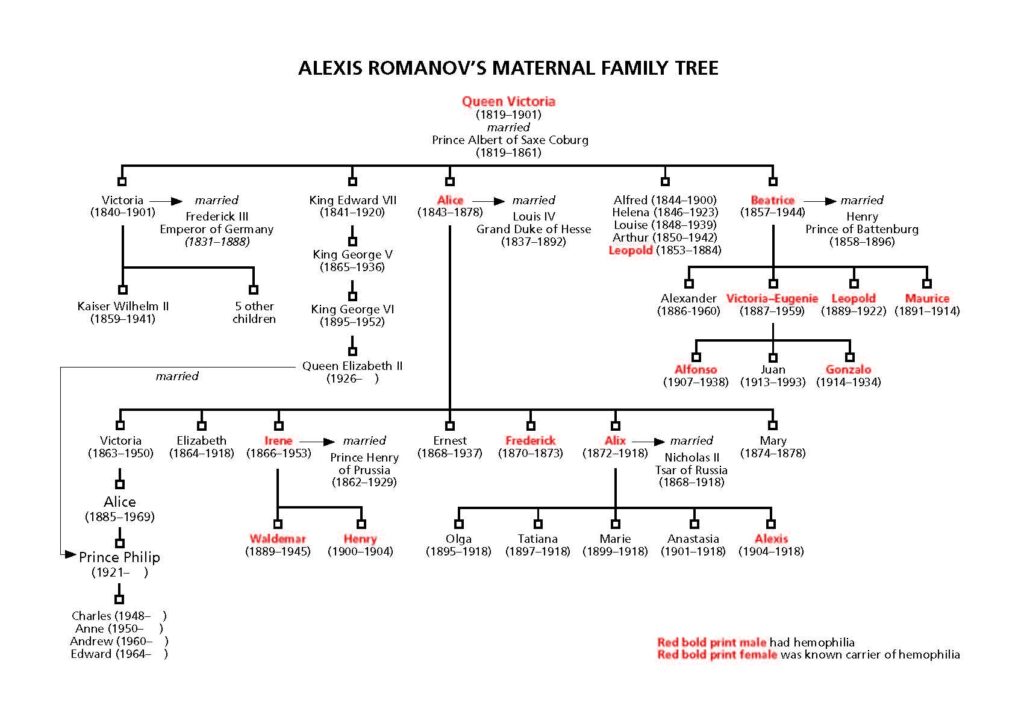
Parents and patients often wonder about the safety of their factor product. Our community suffered terrible losses from contamination of the nation’s blood supply in the 1970s and 80s, so safety is paramount for us. But we often confuse purity and safety when describing factor concentrates. Purity and safety often go hand-in-hand, but in a medical context they have very specific meanings.
Purity: a measure of the presence of other proteins, sometimes including other clotting factors, in addition to the specific factor supplied in the concentrate
Safety: the removal or inactivation of potentially harmful substances, including blood-borne viruses, from factor concentrate
So purity refers to how much of your factor concentrate contains just factor, with no other proteins. Safety refers to reducing the risk of viral transmission.
Purity is measured by specific activity, the ratio of the desired clotting factor protein to the total protein in the concentrate, minus any added albumin (a blood plasma protein).

How is factor purified? That is, how are extraneous proteins removed from factor? By a manufacturing process called chromatography. In simple terms, chromatography involves passing a mixture containing factor through a column (like a glass tube). The column normally contains small beads coated with a substance that attracts the factor and removes it from the mixture. The column is then flushed out to release the factor, resulting in a final mixture that is thousands of times higher in purity and more concentrated than the original mixture.
Please don’t be misled by the term intermediate! These products are still of high purity, although not as high as the ultrapure or monoclonal ones. And note that the various purity levels do not mean there is any less quality control or consistency in manufacturing. Recombinant products are not produced from human blood plasma. They are produced in large stainless steel tanks, called bioreactors, which contain trillions of cells. Into each of these cells, a gene for human factor has been inserted, or “recombined”—the origin of the name recombinant. These genes produce human factor and release it into the culture medium—a nutritious liquid that keeps the
animal (or host) cells alive and growing. Although the source material is not blood, some recombinant products contain extraneous human or animal proteins introduced during the production process or added to the final product.
Next week: What do different generations mean?
Excerpted from Raising a Child with Hemophilia by Laureen A. Kelley.